Why Fixing Your Sleep Could Be Your Body’s Early Warning System
We all know poor sleep feels awful—but what if it’s more than just fatigue? Disrupted rest might be your body quietly signaling early signs of deeper health imbalances. I’m not talking about dramatic symptoms, but subtle red flags like restless nights or unrefreshing sleep. These can precede conditions like metabolic issues, mood disorders, or weakened immunity. What’s wild? Small, consistent changes can make a real difference. Let’s unpack how upgrading your sleep isn’t just about feeling rested—it could be one of the smartest preventive moves you ever make.
The Silent Signal: When Sleep Problems Whisper Before Illness Shouts
Sleep disturbances often emerge long before a formal diagnosis is made. Many people dismiss occasional insomnia or fragmented sleep as normal stress reactions, but these disruptions can be early warnings of underlying physiological imbalances. Research consistently shows that chronic sleep difficulties correlate with a higher likelihood of developing conditions such as hypertension, insulin resistance, and mood disorders. For instance, individuals who regularly experience trouble falling or staying asleep are more likely to show early markers of cardiovascular strain, even when they appear otherwise healthy. These subtle shifts in sleep architecture—such as reduced deep sleep or frequent nighttime awakenings—can reflect changes in brain activity, hormone levels, and nervous system regulation.
One of the most telling patterns is non-restorative sleep, where a person sleeps for a full night but wakes up feeling unrefreshed. This symptom is frequently reported by individuals who later develop chronic fatigue syndrome, fibromyalgia, or metabolic syndrome. Similarly, waking up multiple times during the night, especially around the same hour, may point to hormonal fluctuations or blood sugar instability. While these symptoms alone do not confirm any condition, they serve as physiological signposts—gentle nudges from the body that something may need attention. The key is not to panic but to recognize these signals as opportunities for early intervention.
Women between the ages of 30 and 55 may be particularly sensitive to these early cues. Hormonal transitions such as perimenopause can influence sleep quality, but poor sleep can also exacerbate hormonal imbalances in a feedback loop. This makes it even more important to pay close attention to changes in sleep patterns during midlife. Recognizing these early signs allows for lifestyle adjustments that can support long-term health, potentially delaying or even preventing the onset of more serious conditions. Sleep, in this sense, becomes less of a passive state and more of a diagnostic window into overall well-being.
Why Sleep Isn’t Just Downtime—It’s Maintenance Mode
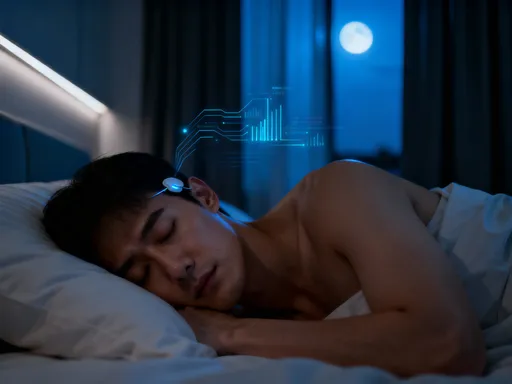
Sleep is not merely a period of rest; it is a biologically active phase during which the body performs essential maintenance. During deep sleep, the brain clears out metabolic waste through the glymphatic system, a process believed to reduce the risk of neurodegenerative diseases. At the same time, the body repairs tissues, synthesizes proteins, and strengthens the immune system. This nightly reset is crucial for maintaining cellular health and preventing the accumulation of damage that can lead to chronic illness. When sleep is consistently disrupted, these restorative processes are compromised, leaving the body more vulnerable to stress, infection, and long-term disease.
Hormonal regulation is another critical function that occurs during sleep. Melatonin, the hormone that signals darkness and promotes sleep onset, also acts as a powerful antioxidant and immune modulator. Cortisol, the stress hormone, follows a natural rhythm that should peak in the morning and taper off at night. Poor sleep can flatten this rhythm, leading to elevated nighttime cortisol levels, which in turn disrupts melatonin production and further impairs sleep. This imbalance not only makes it harder to fall asleep but also contributes to increased inflammation, weight gain, and insulin resistance over time.
Glucose metabolism is similarly affected by sleep quality. Studies have shown that even a few nights of partial sleep deprivation can reduce insulin sensitivity, mimicking early stages of type 2 diabetes. The body’s ability to regulate blood sugar depends heavily on adequate rest, making sleep a foundational pillar of metabolic health. When sleep is compromised, the body struggles to manage energy efficiently, often leading to cravings for high-carbohydrate foods and increased fat storage, particularly around the abdomen. Therefore, improving sleep is not just about feeling more alert—it is about supporting the body’s fundamental regulatory systems that keep it functioning optimally.
Spotting the Patterns: What Your Sleep Is Trying to Tell You
Different types of sleep disruptions can reflect different underlying issues. For example, waking up consistently between 2 a.m. and 4 a.m. may indicate an overactive stress response. During these hours, the body typically experiences a natural dip in core temperature and cortisol levels. If stress hormones remain elevated due to chronic anxiety or poor stress management, they can trigger awakenings. This pattern is common among individuals with high psychological load—those juggling work, family, and caregiving responsibilities—making it especially relevant for middle-aged women who often serve as primary caregivers.
Snoring or gasping during sleep may point to breathing difficulties, such as obstructive sleep apnea, a condition that disrupts oxygen flow and increases cardiovascular risk. While snoring is often dismissed as a minor annoyance, it can be a sign of airway restriction that places strain on the heart and brain over time. Other signs, such as teeth grinding or restless leg syndrome, may be linked to nutrient deficiencies, nervous system dysregulation, or circulatory issues. Recognizing these patterns does not mean self-diagnosing, but rather becoming more attuned to the body’s signals and understanding when to seek professional insight.
Tracking sleep habits can be a powerful tool in identifying trends. Keeping a simple sleep journal—recording bedtime, wake time, nighttime awakenings, and how one feels in the morning—can reveal patterns that might otherwise go unnoticed. Over time, this data can help distinguish between temporary stress-related disruptions and more persistent issues that may require medical evaluation. The goal is not perfection but awareness. By paying attention to sleep quality, individuals gain valuable insight into their overall health and can take proactive steps before symptoms escalate.
The Simple Shifts That Actually Work (No Gimmicks)
Improving sleep does not require expensive supplements or drastic lifestyle changes. Some of the most effective strategies are simple, accessible, and grounded in science. One of the most powerful habits is maintaining a consistent sleep schedule—even on weekends. Going to bed and waking up at the same time every day helps regulate the body’s internal clock, making it easier to fall asleep and wake up naturally. This consistency strengthens circadian rhythms, which in turn supports hormone balance, mood stability, and energy levels throughout the day.
Reducing exposure to blue light in the evening is another highly effective practice. Devices such as smartphones, tablets, and televisions emit blue wavelengths that suppress melatonin production, delaying sleep onset. Limiting screen time at least one hour before bed—or using blue light filters—can significantly improve sleep quality. Instead, engaging in calming activities such as reading a physical book, listening to soft music, or practicing gentle stretching can signal to the body that it’s time to wind down. These routines create a psychological transition from wakefulness to sleep, reducing mental arousal and promoting relaxation.
Mindful wind-down routines can also make a meaningful difference. Taking a warm bath, sipping herbal tea like chamomile or passionflower, or practicing deep breathing exercises can activate the parasympathetic nervous system, which promotes calmness. These practices don’t need to be elaborate—just consistent. Over time, the brain begins to associate these activities with sleep, making it easier to drift off. The key is sustainability: small changes that fit naturally into daily life are more likely to become lasting habits than extreme measures that feel burdensome.
Your Bedroom as a Health Lab: Environment Matters More Than You Think
The sleep environment plays a crucial role in determining sleep quality. A bedroom that is too warm, noisy, or bright can interfere with the body’s ability to enter and maintain deep sleep stages. Research shows that the ideal sleep temperature is between 60 and 67 degrees Fahrenheit (15–19°C). A cooler room supports the natural drop in core body temperature that occurs during sleep onset, facilitating faster and more restful sleep. Simply adjusting the thermostat or using breathable bedding can make a noticeable difference.
Light exposure is another critical factor. Even small amounts of light—from street lamps, electronic devices, or digital clocks—can disrupt melatonin production. Using blackout curtains or a sleep mask helps create a dark environment that supports uninterrupted sleep. Similarly, minimizing noise through earplugs, white noise machines, or soundproofing techniques can prevent micro-awakenings that fragment sleep without full consciousness. These subtle disturbances may not wake a person completely, but they reduce sleep efficiency and impair restorative processes.
Decluttering the bedroom and removing electronic devices not only reduces visual and mental stimulation but also limits temptation to check phones or emails at night. A bedroom designed for sleep—comfortable, quiet, cool, and dark—functions like a personal health lab where the body can perform its nightly maintenance without interference. Simple upgrades, such as investing in a supportive mattress or using hypoallergenic pillows, can further enhance comfort and alignment, especially for those with physical discomfort or allergies. When the environment supports sleep, the body responds with deeper, more restorative rest.
When to Lean In—And When to Call a Pro
While many sleep issues can be improved with lifestyle changes, some symptoms warrant professional evaluation. If a person experiences frequent gasping, choking, or pauses in breathing during sleep, it could indicate sleep apnea, a condition that requires medical diagnosis and treatment. Similarly, persistent fatigue despite adequate sleep, excessive daytime sleepiness, or involuntary limb movements at night should be discussed with a healthcare provider. These symptoms may point to underlying sleep disorders or other medical conditions that cannot be resolved through self-care alone.
It’s also important to seek help if insomnia persists for more than a few weeks, especially if it affects daily functioning, mood, or concentration. Chronic insomnia can contribute to anxiety, depression, and reduced quality of life, but effective treatments—including cognitive behavioral therapy for insomnia (CBT-I)—are available. A healthcare provider can help rule out medical causes such as thyroid dysfunction, anemia, or medication side effects that may be impacting sleep.
Self-care and professional care are not mutually exclusive—they are complementary. Taking steps to improve sleep hygiene shows initiative and commitment to health, but knowing when to seek expert guidance ensures that serious issues are not overlooked. Open conversations with doctors about sleep concerns can lead to timely interventions and better outcomes. The goal is not to manage everything alone, but to build a support system that includes both personal effort and professional insight.
Sleep as Prevention: A Long-Term Investment in Well-Being
Viewing sleep as preventive healthcare reframes it from a luxury to a necessity. Just as regular exercise and a balanced diet are pillars of long-term health, so too is consistent, high-quality sleep. Every night offers an opportunity to support the body’s natural repair mechanisms, regulate hormones, and strengthen immunity. Over time, these nightly investments accumulate, reducing the risk of chronic diseases such as heart disease, diabetes, and cognitive decline. For women in midlife, prioritizing sleep can ease the transition through hormonal changes and support emotional resilience.
The benefits extend beyond physical health. Restorative sleep enhances mood, improves decision-making, and increases patience and presence in daily life. It allows for greater enjoyment of family, work, and personal interests. When energy is stable and mental clarity is improved, even routine tasks feel more manageable. This ripple effect underscores the profound impact that sleep has on overall quality of life.
Listening to your sleep is one of the simplest yet most powerful acts of self-care. It requires no special equipment, no prescriptions, and no drastic changes—just attention and intention. By tuning in to sleep patterns, making small adjustments, and seeking help when needed, individuals take meaningful steps toward a healthier future. In a world that often glorifies busyness and sacrifice, choosing to prioritize sleep is a quiet act of strength. It is a promise to oneself: to rest deeply, live fully, and protect well-being—one night at a time.