How I Tamed My Cholesterol Without Medication — Real Life Changes That Worked Fast
Ever feel like your blood test results are speaking a foreign language? I did — until my doctor flagged high cholesterol and I realized I couldn’t ignore it anymore. The good news? Small, consistent lifestyle shifts made a noticeable difference in weeks, not years. This isn’t about extreme diets or magic pills. It’s about real, doable habits that actually work. Let me walk you through what changed for me — and how it can help you too. Always consult your doctor, though — this is my journey, not medical advice.
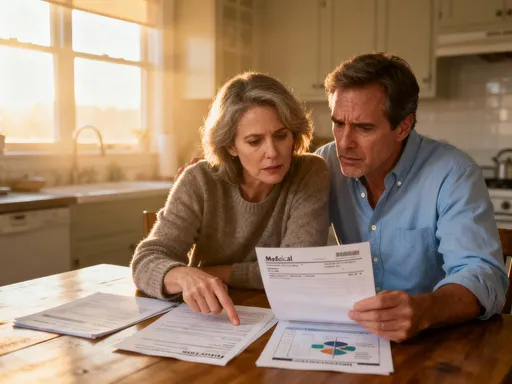
The Wake-Up Call: When My Lipid Panel Shocked Me
It started with a routine check-up. I walked into the clinic feeling perfectly fine — no chest pain, no fatigue, no warning signs. I was eating what I thought was a balanced diet, walking occasionally, and managing my busy life as best I could. So when my doctor called a few days later and said, “Your LDL is high,” I was stunned. I didn’t even know what LDL meant.
That conversation was my wake-up call. My total cholesterol was 245 mg/dL, with LDL (low-density lipoprotein) at 160 mg/dL — well above the recommended level of 100 mg/dL. My triglycerides were also elevated, and my HDL (high-density lipoprotein), the “good” cholesterol, was too low. The numbers painted a picture I couldn’t ignore: my arteries could be silently accumulating plaque, increasing my risk for heart disease — and I wouldn’t feel it until it was too late.
What surprised me most was that high cholesterol doesn’t announce itself. There are no symptoms, no alarms. It’s a quiet, invisible threat. Yet, according to the Centers for Disease Control and Prevention (CDC), nearly 94 million adults in the U.S. have high total cholesterol, and only about half are managing it effectively. The danger lies in its stealth — by the time symptoms appear, such as chest discomfort or reduced stamina, significant damage may already be done.
That moment shifted my mindset. I didn’t want to wait for a crisis. I wanted to act — not out of fear, but out of care for my long-term health. My doctor didn’t immediately prescribe medication, but made it clear: if I didn’t make changes, it would likely be the next step. That gave me motivation. I decided to try a natural, lifestyle-first approach. I wanted to see if real, sustainable habits could bring those numbers down — and they did.
Why Lifestyle Is Your First Line of Defense
Many people assume that high cholesterol means a prescription is inevitable. But research consistently shows that lifestyle changes are not just supportive — they are foundational. In fact, the National Lipid Association emphasizes that therapeutic lifestyle changes should be the starting point for anyone with elevated cholesterol, regardless of risk level.
Your liver produces most of your cholesterol, but what you eat, how you move, and how well you sleep directly influence how it functions. Dietary saturated fats — found in red meat, full-fat dairy, and processed snacks — signal the liver to produce more LDL. Meanwhile, trans fats, often hidden in packaged baked goods, are even worse, raising LDL while lowering HDL. On the flip side, unsaturated fats from plants and fish can help improve your lipid profile.
Insulin sensitivity also plays a role. When cells become resistant to insulin — often due to excess sugar and refined carbohydrates — the body stores more fat, including in the bloodstream as triglycerides. This metabolic shift contributes to what’s known as “dyslipidemia,” an unhealthy pattern of cholesterol and fats that increases cardiovascular risk.
Here’s the encouraging part: unlike medication, which works on specific pathways, lifestyle changes address the root causes. And the timeline for results? Much faster than many assume. Clinical studies show that meaningful improvements in LDL and triglycerides can occur within 4 to 8 weeks of consistent changes. One meta-analysis published in the Journal of the American Heart Association found that dietary and exercise interventions reduced LDL by an average of 15–20% in just six weeks. That’s not years — that’s less than two months.
Of course, medication has its place, especially for those with genetic conditions like familial hypercholesterolemia or established heart disease. But for many, a dedicated effort to improve daily habits can delay or even eliminate the need for statins. The key is consistency — not perfection.
What I Changed in My Daily Routine (And Why It Mattered)
I started by auditing my plate. I thought I ate well, but when I looked closely, my meals were heavy in refined carbohydrates — white bread, pasta, sugary cereals — and low in fiber. I also used butter regularly and snacked on cheese and crackers in the evenings. These habits, common among busy adults, were quietly working against my cholesterol.
My first change was simple: swap refined grains for whole grains. I switched to oatmeal for breakfast, choosing steel-cut or old-fashioned oats instead of instant. Oats are rich in beta-glucan, a type of soluble fiber proven to reduce LDL cholesterol by binding to bile acids in the gut and helping the body excrete them. I also started eating quinoa, brown rice, and whole grain bread, which kept me fuller longer and stabilized my energy.
Next, I rethought my fats. I replaced butter with extra virgin olive oil for cooking and dressings. I added a handful of raw almonds or walnuts to my daily routine and began slicing avocado onto salads and sandwiches. These foods are high in monounsaturated and polyunsaturated fats — the kind that support heart health. The Portfolio Diet, studied extensively by researchers at the University of Toronto, combines these foods with plant sterols, soy protein, and soluble fiber, showing LDL reductions comparable to low-dose statins.
I also increased my intake of legumes — beans, lentils, chickpeas — which are packed with both protein and soluble fiber. A cup of cooked lentils provides about 15 grams of fiber, nearly half the daily recommended amount. I started adding beans to soups, making hummus for snacks, and trying meatless meals once or twice a week.
Sugar was another target. I cut out soda and switched to sparkling water with lemon. I stopped buying fruit juices, even “100% natural” ones, which can contain as much sugar as soda. Instead, I ate whole fruits — apples, pears, berries — which provided fiber and antioxidants without the blood sugar spikes. Hydration became a priority too; I aimed for eight glasses of water daily, which helped reduce bloating and curb unnecessary snacking.
The Movement Hack That Actually Fit My Schedule
I used to think exercise had to be intense to matter. I’d sign up for fitness classes, go all-in for a week, then burn out. The cycle left me discouraged. This time, I focused on sustainability. I committed to 30 minutes of brisk walking five days a week — something I could actually maintain.
Walking might sound modest, but it’s powerful. Research from the American College of Cardiology shows that regular moderate-intensity exercise like brisk walking improves HDL levels and lowers triglycerides. It also enhances insulin sensitivity, helping the body manage blood sugar and fat storage more efficiently. Within three weeks, I noticed I could walk faster and farther without getting winded. My sleep improved, and I felt more alert during the day.
Twice a week, I added short resistance sessions using just my body weight. Ten minutes of squats, wall push-ups, and step-ups in the evening made a difference. Strength training builds muscle, and muscle tissue burns more calories at rest, which supports metabolic health. Over time, this contributes to better lipid metabolism. I didn’t need a gym or equipment — just consistency.
The beauty of this routine was its flexibility. On busy days, I walked during phone calls or after dinner. On weekends, I turned walks into family outings — a change that brought us closer while supporting my health. Movement stopped being a chore and became a part of my day, like brushing my teeth. And the results showed: after six weeks, my follow-up lab work revealed a 12% drop in LDL and a noticeable rise in HDL.
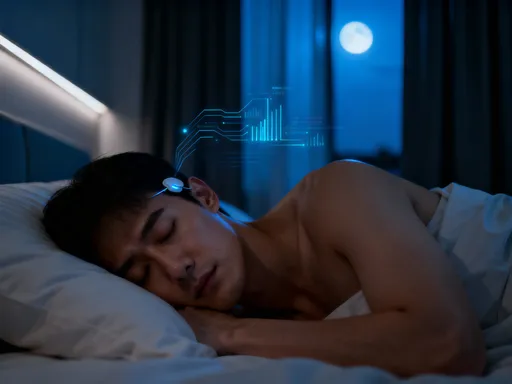
Sleep and Stress: The Hidden Cholesterol Triggers I Ignored
I didn’t realize how much my sleep — or lack of it — was affecting my cholesterol. I was averaging about six hours a night, often lying awake worrying about work or family responsibilities. I drank coffee late in the day and scrolled through my phone in bed, habits that disrupted my natural sleep cycle.
Chronic poor sleep and stress are silent contributors to dyslipidemia. When the body is under stress, it releases cortisol, a hormone that increases blood sugar and promotes fat storage, particularly around the abdomen. Elevated cortisol also disrupts lipid metabolism, raising LDL and triglycerides while lowering HDL. A study in the journal Sleep found that adults who slept less than six hours per night had higher total cholesterol and lower HDL than those who slept seven to eight hours.
I knew I had to change this. I set a bedtime of 10:30 p.m. and created a wind-down routine: no screens after 9:30, a cup of caffeine-free herbal tea (chamomile or passionflower), and five minutes of deep breathing or light stretching. I also stopped checking emails after dinner. These small shifts helped me fall asleep faster and stay asleep longer.
Within four weeks, I was consistently getting seven to eight hours. The impact was remarkable — not just on my cholesterol, but on my mood and energy. I felt calmer, more focused, and less reactive to daily stressors. When I retested, my triglycerides had dropped by 18%, a change my doctor noted with approval. Sleep and stress management weren’t side notes — they were central to my success.
Tracking Progress Without Obsession: My Simple Monitoring System
I didn’t want to become obsessed with numbers, but I did want to stay accountable. I started a simple food journal, logging meals and noting how I felt afterward — energized, sluggish, satisfied. I didn’t track every calorie, but I paid attention to patterns. For example, I noticed that days with more vegetables and whole grains left me feeling lighter and more productive.
I avoided stepping on the scale every day. Weight can fluctuate for many reasons, and I didn’t want short-term changes to derail my motivation. Instead, I focused on non-scale victories: my clothes fit better, I had more energy, and I wasn’t reaching for snacks out of boredom or stress.
Most importantly, I scheduled a follow-up blood test at six weeks. This was the real measure of progress. When the results came back, I was thrilled: total cholesterol down to 202 mg/dL, LDL at 128 mg/dL, and HDL up by 5 points. Triglycerides had improved significantly. My doctor said the changes were impressive and encouraged me to keep going.
I learned that progress isn’t linear. Some weeks I slipped — a birthday party with cake, a stressful week with less sleep. But I didn’t let those moments undo my efforts. I returned to my habits without guilt. Consistency, not perfection, was the goal. Over time, the positive changes became automatic, part of my identity rather than a temporary fix.
Putting It All Together: A Sustainable Plan, Not a Quick Fix
Looking back, no single change transformed my cholesterol overnight. It was the combination — better food choices, regular movement, improved sleep, and stress reduction — that created real results. These habits didn’t just lower my numbers; they improved my overall quality of life. I had more energy, better focus, and a renewed sense of control over my health.
What made this approach work was that it was sustainable. I didn’t cut out foods I loved completely — I just enjoyed them in moderation. I didn’t force myself into grueling workouts — I found movement I enjoyed. I treated myself with kindness, not criticism. This wasn’t a diet; it was a lifestyle shift built on self-care.
If you’re facing high cholesterol, know this: you have more power than you think. Start with one small change — swap white rice for brown, take a 15-minute walk after dinner, or go to bed 30 minutes earlier. Master that, then add another. Small steps compound into big results. The habits that lower cholesterol also reduce the risk of diabetes, high blood pressure, and other chronic conditions.
Always remember to work with your healthcare provider. This journey is personal, and medical guidance is essential, especially if you have other health conditions. But know that lifestyle is not a substitute for medicine — it’s the foundation upon which medicine, if needed, can build.
High cholesterol doesn’t have to be a life sentence. With informed choices and daily commitment, it can be managed — often without medication. My story isn’t unique. It’s proof that real, lasting change is possible when you align your habits with your health. You don’t need perfection. You just need to begin.